Clinical Biochemistry

How Does Clinical Biochemistry Work?
Most clinical biochemistry laboratories provide two distinct types of diagnostic testing – clinical chemistry and immunoassays – using large, fully automated analyzers. These instruments are either manually loaded or mechanically fed with patient sample tubes – usually whole blood or serum, but also sputum, urine or feces – providing end-to-end processing and analysis without further user interaction. Most clinical chemistry tests rely on colorimetric methods or ion selectiveelectrode technologies, whereas immunoassays combine an antibody or enzymatic target-recognition element with fluorescence- or luminescence-based readout to allow detection of a broad range of complex biomarkers. These various assay types and detection technologies can either be performed on separate, dedicated instruments or combined on a single high volume platform, depending on assay portfolios and throughput requirements.
What is Clinical Biochemistry used for?
Clinical biochemistry makes up a large proportion of all pathology testing performed in hospitals to aid in the diagnosis and care of patients. There are a huge number of different biomarkers that are routinely tested, depending on the patient’s clinical presentation and history. These range from simple tests to check liver or kidney function, or identify the presence of a drug of abuse, to complex time-course studies looking at hormone imbalance or the efficacy of therapeutic drugs.
Why would you use Clinical Biochemistry?
Testing a patient’s bodily fluids for the presence or absence of specific biomarkers can help to provide a definitive diagnosis of their condition, as well as an indicator of the effectiveness of any treatments being administered.
How does Clinical Biochemistry Work?
Most clinical biochemistry laboratories provide two distinct types of diagnostic testing – clinical chemistry and immunoassays – using large, fully automated analyzers. These instruments are either manually loaded or mechanically fed with patient sample tubes – usually whole blood or serum, but also sputum, urine or feces – providing end-to-end processing and analysis without further user interaction. Most clinical chemistry tests rely on colorimetric methods or ion selective electrode technologies, whereas immunoassays combine an antibody or enzymatic target-recognition element with fluorescence- or luminescence-based readout to allow detection of a broad range of complex biomarkers. These various assay types and detection technologies can either be performed on separate, dedicated instruments or combined on a single high volume platform, depending on assay portfolios and throughput requirements.
What is Clinical Biochemistry used for?
Clinical biochemistry makes up a large proportion of all pathology testing performed in hospitals to aid in the diagnosis and care of patients. There are a huge number of different biomarkers that are routinely tested, depending on the patient’s clinical presentation and history. These range from simple tests to check liver or kidney function, or identify the presence of a drug of abuse, to complex time-course studies looking at hormone imbalance or the efficacy of therapeutic drugs.
Why would you use Clinical Biochemistry?
Testing a patient’s bodily fluids for the presence or absence of specific biomarkers can help to provide a definitive diagnosis of their condition, as well as an indicator of the effectiveness of any treatments being administered.
Because clinical biochemistry is based on testing liquids or suspensions, high quality water is required for almost every step of sample processing, from diluting reagents, samples and detergents to washing reaction vessels and sample probes. Poor water quality can both interfere with the tests themselves – leading to incorrect or misleading results – and affect the general operation of the analyzers, increasing the likelihood of malfunction.
What Types of Contaminants in Water can Affect Clinical Biochemistry Results?
The main types of impurity that affect the performance of clinical biochemistry analyzers are particulates, ions, bacteria and bacterial by-products, and organics.
1. Particulates
Due to the very low volumes of samples and reagents used the presence of particulates during pipetting operations can lead to inconsistent volumes of reagents and/or samples being added to the reaction vessel, reducing both the specificity and sensitivity of assays. In addition, particulates may increase the opacity of the reaction mixture, leading to further reductions in sensitivity.
Insoluble or low solubility particulates can also affect the operation of the analyzer, by blocking capillaries used for liquid transfers, and causing deposits or scaling to form at liquid junctions and boundaries, encouraging bacterial growth and the formation of biofilms.
2. Ions
Ionic contamination leads to a variety of issues, affecting the performance of chemistry tests and immunoassays. For example, ions in the wash water can lead to cross-contamination/carryover, whereas ions in the diluent or standards can affect the stability of reagents, leading to drift over time, and a loss of accuracy. The low resistivity which results from this type of contamination can also lead to the need for more frequent calibration with excessive reagent consumption and wastage, increasing testing times and costs.
3. Bacteria and Bacterial By-Products
The presence of bacteria in analyzer water supplies can impact both overall instrument performance and assay results in a number of ways. Similar to particulates, they cause blockages or deposits throughout the fluid path, reducing the accuracy of liquid transfers and the efficiency of wash systems. Assay performance can also be affected by bacterial growth increasing the opacity of reaction mixtures – decreasing sensitivity – and reducing the stability of samples and reagents. Similarly, Several bacterial by-products can directly interfere with assay chemistries or binding. For example, fluorescein-based dyes released from bacteria such as Pseudomonas aeruginosa can lead to high blanks and out-of-range standards during calibration, as well as false positive results.
4. Organics
A variety of organic compounds can interfere either directly or indirectly with assay performance and detection. The exact mechanism and degree of interference varies significantly depending on the contaminant, analyte and detection method, leading to unpredictable and inconsistent results. For example, carboxylic acids can interfere with enzyme activity and immunoassays by binding to active sites and complexing with co-factor metals. Other organics may inhibit enzymes via different mechanisms, and affect fluorescent detection.
What are the Water Purity Requirements for Clinical Biochemistry?
To avoid the various issues associated with water contamination outlined above, the College of American Pathologists (CAP) – the internationally-recognized body responsible for accreditation of clinical laboratories in the USA – recommends that all water used for any application in laboratory testing should meet the Clinical Laboratory Reagent Water (CLRW) standard specified by CLSI as a minimum. In addition, instrument feed water must meet the instrument manufacturer’s specifications – which may be more rigorous that CLRW standards – to ensure accurate and reproducible results.
CLRW/CLSI Specifications:
The CLRW resistivity specification of >10 MΩ.cm restricts the concentrations of ionic impurities to ppb levels or lower, and requires the elimination of carbon dioxide. This is adequate for most clinical work but, when trace elements need to be determined, the resistivity needs to be much higher – at 18.2 MΩ.cm. Similarly, CLRW relies on filtration to remove particulates, but the 0.2 μm filters specified may not always be adequate with the very low liquid volumes used in modern clinical assays.
The TOC spec of <500 ppb in CLRW is a reflection of earlier standards, and can still lead to the presence of a wide variety of organic compounds – such as carboxylic acids and polyaromatics – which could jeopardize low volume assays. Bacterial contamination also has serious effects on all aspects of analyzer operation, requiring consistently low levels of contamination to avoid biofilm formation and ongoing issues.
Water supplies used for clinical biochemistry must therefore be validated as fit for purpose, and the CLSI emphasizes the need for rigorous trending of water system parameters to ensure that water purity is achieved and maintained.
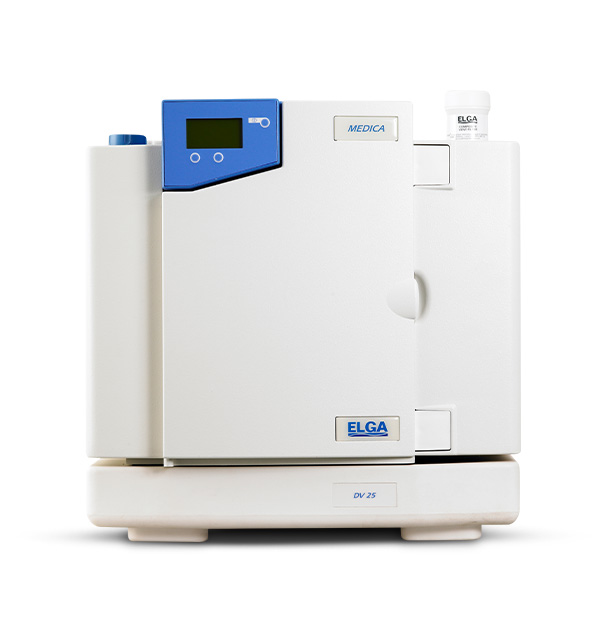
How does ELGA Solve Water Purity Problems for Clinical Biochemistry?
ELGA’s expertise and long-standing reputation ensure that its knowledgeable team can help customers to determine the level of water purity required for their applications. The company offers a range of water purification systems for clinical applications, with each having its own advantages and limitations. For example, the CENTRA® range of centralized purification and distribution systems has revolutionized the way that large volumes of pure water are produced, stored and distributed in clinical laboratories. The CENTRA R-200 is a complete water purification, storage, control, and distribution system providing Type I (Ultrapure), Type II and Type III pure water, with a 200 liters per hour reverse osmosis module and 0.2 μm filters.
Conclusion
The purity of instrument feed water is crucial for the smooth and consistent operation of fully automated clinical chemistry and immunoassay analyzers. The combination of high throughput instrumentation and high sensitivity, low volume assays requires water of very high purity, with minimal particulate, ionic, organic, bacterial and bacterial by-product content to ensure the long term accuracy of results. ELGA’s broad range of water purification systems helps clinical laboratories around the world to ensure that patient testing is not affected by water impurities.